Gynecomastia
Male chest contouring, also called gynecomastia surgery or male breast reduction, removes excess fat and glandular tissue to sculpt a flatter and more masculine chest.

Gynecomastia surgery—also known as male breast reduction—is a cosmetic procedure that removes excess fat and overdeveloped breast tissue in men. This condition, called gynecomastia, can cause the chest to appear rounder or more feminine, sometimes with noticeable puffiness or enlargement of the areola.
Male chest surgery typically includes a combination of:
• Liposuction to reduce fatty tissue
• Excision of dense glandular breast tissue
The goal is to restore a flatter, firmer, and more proportionate chest shape with minimal visible scarring.
What you need to know
Every procedure and treatment we offer is thoughtfully designed to meet your unique goals, lifestyle, and anatomy. Below, you’ll find key details about what to expect—from how the procedure works to recovery guidance and ideal candidacy—so you can feel informed, confident, and empowered at every step of your journey.
Surgery length: 2–3 hours
Anesthesia: Local (awake) or general anesthesia (asleep)
Setting: Outpatient procedure (go home same day)
Drains: Rarely required
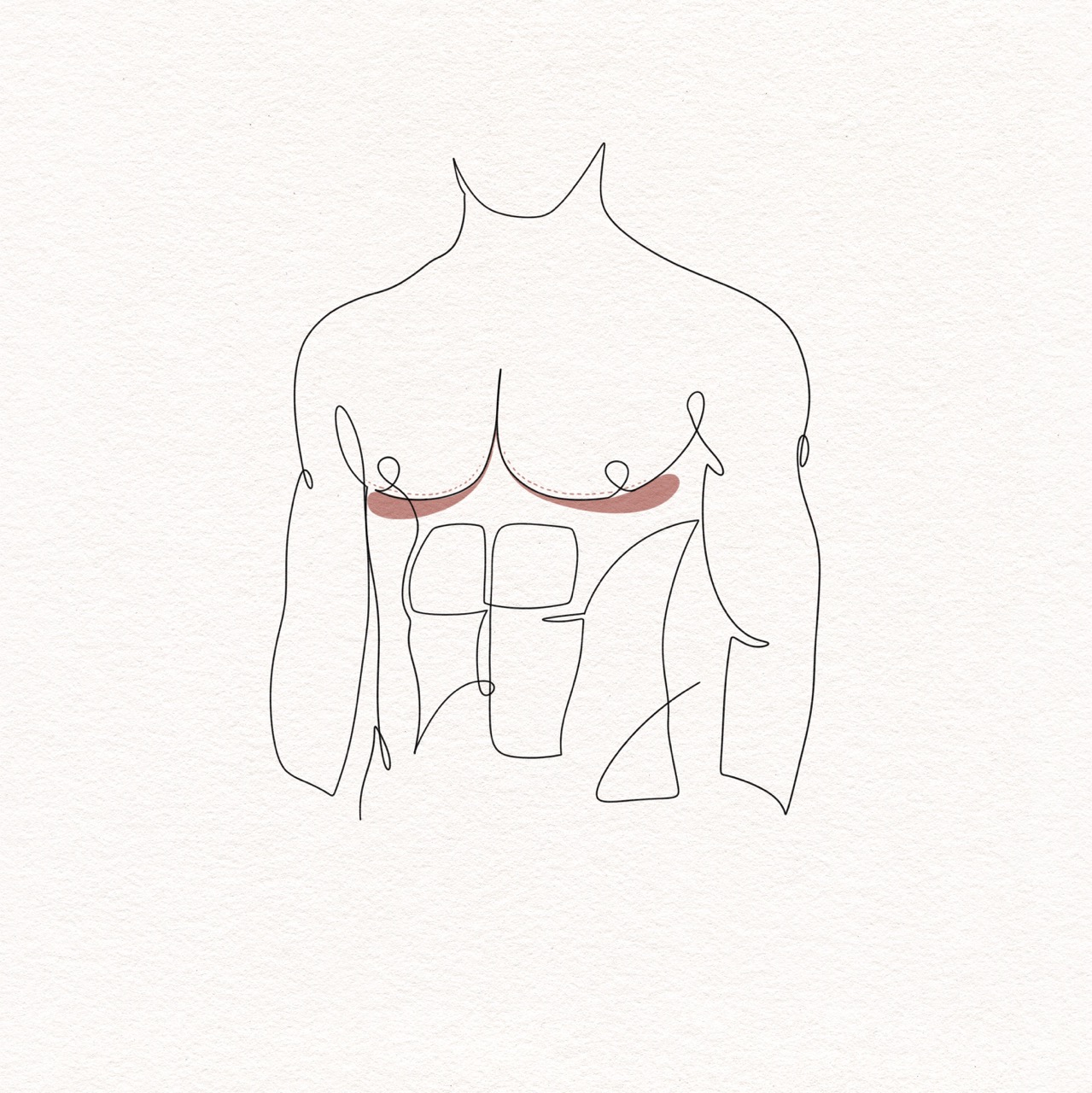
Incisions: Small scars at the edge of the areola and outer chest wall
Recovery time: 1-2 weeks for light activity
Reduces enlarged or puffy male breast tissue
Restores a more masculine chest shape and definition
Improves nipple and areola proportion and contour
Decreases physical discomfort, tenderness, or tightness
Boosts confidence in fitted clothing and shirtless settings
You may be a good candidate for male chest surgery if you:
Are in overall good health
Do not smoke or use nicotine products or are willing to stop using these products for a time
Are at a stable weight
Have enlarged glandular tissue and/or chest fat
Experience puffiness or tenderness in the chest
Are bothered by the appearance of your chest and desire a more defined, masculine contour

An overview of the procedure
View our Before & After Gallery
Scroll through our extensive gallery showcasing the transformations of real patients from Metropolitan Plastic Surgery.


Every person is unique and may have some similarities as well as differences to others in terms of their individual recovery experience. A mommy makeover is a combination of multiple procedures so it is common to have more downtime and required healing than if these procedures were performed individually.

Day of Procedure
Return home the same day (outpatient surgery).
A compression garment will be placed over your chest to minimize swelling and support healing.
Mild to moderate discomfort is expected, usually well managed with prescription pain and anti-inflammatory medications.
Change dressings. Some drainage from incision sites is expected.

Days 1-3
Swelling, bruising, and mild discomfort are common and may peak during this time.
Gentle walking is encouraged to maintain circulation, but strenuous activity must be avoided.
Take first shower and change dressings.
Keep the compression garment on at all times except with bathing or washing the garment.

Weeks 1-2
Most patients return to non-physical work within 3–7 days.
Pain significantly decreases by the end of week one.
Return for your first post-op appointment.
Shower and wash garment daily.
Continue wearing your compression garment 24/7.

Weeks 2-4
Swelling and bruising continue to subside.
Light cardio (like walking or stationary cycling) may be allowed if cleared by Dr. Aimé.
Continue wearing the compression garment.
Incisions continue to heal.

Weeks 4-6
Most restrictions are lifted around this time, including returning to moderate strength training or more active workouts.
May discontinue wearing compression garment.
Final results begin to appear as residual swelling decreases.
Massage and scar care may be recommended depending on your healing progress.

After Week 6
The majority of swelling will resolve over 3-6 months and your chest will have a more natural appearance.
Scar maturation will continue for one year—sun protection is crucial to prevent hyperpigmentation.
You can return to full physical activity, including chest workouts, overhead lifting and getting the pool.
You'll continue to follow-up with Dr. Aimé to ensure proper healing.
Final results are typically assessed between 6-12 months post-op.
"I was very pleased with Dr. Aimé because she made me feel comfortable by explaining her methods in a conversational manner. I couldn’t be happier with my result. I highly recommend Dr. Aimé!"
“I recently underwent a submentoplasty procedure performed by the incredibly talented plastic surgeon, Dr Aimé. My decision to have submentoplasty was not taken lightly and Dr Aimé made sure to thoroughly explain the entire procedure to me during our consultation.”
Frequently Asked Questions
We’ve gathered answers to some of the most common questions our patients ask about this procedure. Whether you’re just starting your research or preparing for surgery, this section is here to help you feel informed and confident every step of the way.
There are many causes of gynecomastia. Lifestyle choices such as poor diet and lack of exercise can lead to increased fatty tissue over the chest. Hormone fluctuations (such as during puberty), anabolic steroids and testosterone supplementation can stimulate enlargement of the breast tissue. Many medications (such as sprinolactone, ketoconazole, and cimetidine) as well as recreational drugs, including marijuana, can also cause gynecomastia. Medical conditions including liver disease, thyroid disease, kidney disease and certain cancers such as testicular cancer are also associated with gynecomastia. In some cases the cause of gynecomastia remains unknown.
Gynecomastia is quite common. It is not unusual for men to feel that they are the only one with this condition. Many men wear compression undershirts and avoid shirtless situations such as the beach or the pool due to distress and embarrassment from the appearance of their chest. However, gynecomastia is more common than is typically discussed. There are generally three peaks during a lifespan that gynecomastia occurs. The first is during infancy due to estrogens in breast milk. The second most common timeframe to develop gynecomastia is during puberty. In fact, up to 70% of male adolescents develop gynecomastia due to hormonal changes during puberty and 25% of the time this pubertal gynecomastia does not resolve on its own and persists into adulthood. The last most common timeframe to develop gynecomastia is middle age to early older age, in which up to 65% of men are affected. So although not commonly openly discussed, gynecomastia is in fact very common.
Generally, no. Most gynecomastia is a benign process that is mostly just emotionally distressing and not in itself harmful. During your consultation appointment, your medical history will be thoroughly reviewed and a physical exam will be performed. Only if there are any concerning findings, which is quite rare, will Dr. Aime recommend follow-up with your primary care doctor for further work-up imaging or labs prior to your procedure.
Yes, it can in most cases. Often, patients choose to have liposuction done on other areas (such as the armpits, neck, abdomen or flanks) or a tummy tuck performed during the same surgery.
Yes, any excised male breast gland is sent to pathology to ensure that there are no masses present within the tissue. While male breast cancer is very rare, it does exist and it is important to have a pathologist review the removed glandular tissue to ensure that it is not present.
The most common complication after male chest surgery is accumulation of blood under the skin of the chest (called a hematoma). Although this can require that the wound is opened to drain the fluid, it can often be treated with needle aspiration in the office and additional compression. Loss of sensation of the nipple and areola is uncommon, but can occur. Although rare, the blood supply to the nipple and areola can be injured during the procedure resulting in loss of viability of the areolar skin. This can possibly require an additional procedure to reconstruct the nipple areola or medical tattooing to restore the natural pigment, which can be faded (called hypopigmentation) in rare cases.
Generally, the results from male chest surgery are long-lasting. Weight gain, steroid use (testosterone or anabolic steroids), certain medications, marijuana use, hormone fluctuation and some medical conditions can lead to recurrence of gynecomastia. A small amount of male breast gland is left under the nipple and areola purposely during the procedure to support the nipple and areola and prevent it from "caving in."
True gynecomastia, where the breast tissue itself is enlarged, will not typically go away with weight loss and exercise. The most effective treatment for gynecomastia is surgery to remove the enlarged breast tissue.
However, pseudogynecomastia, which is when the enlarged breasts are made up of only fatty tissue, which is most commonly seen in older or over-weight men, may improve with weight loss and exercise.
Ready to start your transformation?
Whether you’re just beginning to explore your options or have specific goals in mind, we’re here to guide you with expertise and compassion.

Read more articles

Body Contouring for Men
Body contouring for men is a customized approach to reduce stubborn fat, tighten loose skin, and define masculine features—giving you a leaner, stronger silhouette.

Face & Neck Rejuvenation for Men
Discover tailored solutions for men seeking a more youthful, confident appearance. Our Face & Neck Rejuvenation for Men services focus on enhancing masculine features while addressing visible signs of aging. Explore surgical and non-surgical options designed to deliver natural-looking results that help you look as strong and vital as you feel.