Breast Reduction
Experience relief from discomfort and feel confident in your body with breast reduction surgery in Scottsdale, performed by Dr. Victoria Aimé.

Breast reduction surgery, or reduction mammoplasty, is a highly effective procedure designed to reduce the size, volume, and weight of the breasts. Ideal for individuals experiencing physical discomfort, activity limitations, or emotional distress from overly large breasts, this surgery removes excess breast tissue, skin, and fat while reshaping the remaining breast for a lifted, proportional appearance. The nipple and areola are repositioned to a more youthful location, and the areola can be resized if desired. Patients often report significant improvement in back, neck, and shoulder pain—along with a boost in confidence and overall quality of life.
What you need to know
Every procedure and treatment we offer is thoughtfully designed to meet your unique goals, lifestyle, and anatomy. Below, you’ll find key details about what to expect—from how the procedure works to recovery guidance and ideal candidacy—so you can feel informed, confident, and empowered at every step of your journey.
3–5 hour surgery length
General anesthesia
Outpatient procedure (unless combined with other surgeries)
Drains typically not required
Scars placed around the areola, vertically down the breast, and along the lower breast crease
Recovery time: 2–4 weeks for light activity
Reduces excess breast tissue and skin
Lifts and reshapes sagging breasts
Repositions the nipple and areola to a more aesthetic position
Improves breast symmetry
Alleviates back, neck, and shoulder pain
Improves fit and comfort in clothing and bras
Enhances mobility and freedom during physical activity
You may be a good candidate for breast reduction surgery if you:
Are in overall good health
Do not smoke or are willing to quit nicotine products
Are at a stable weight for at least 6 months
Experience physical discomfort, limited activity, or self-consciousness due to large breasts
Have realistic expectations and a desire for better body balance and quality of life

An overview of the procedure
View our Before & After Gallery
Scroll through our extensive gallery showcasing the transformations of real patients from Metropolitan Plastic Surgery.


"She explained the process and procedures extensively to me and was always available for any questions I may have had. I went into surgery and recovery feeling safe, confident, and comfortable thanks to Dr. Aimé. I am extremely happy with my results and have complete trust in her. I will continue to use her for any future procedures or treatments and I highly recommend Dr. Aimé to anyone considering plastic surgery!"
“I recently underwent a submentoplasty procedure performed by the incredibly talented plastic surgeon, Dr Aimé. My decision to have submentoplasty was not taken lightly and Dr Aimé made sure to thoroughly explain the entire procedure to me during our consultation.”
Frequently Asked Questions
We’ve gathered answers to some of the most common questions our patients ask about this procedure. Whether you’re just starting your research or preparing for surgery, this section is here to help you feel informed and confident every step of the way.
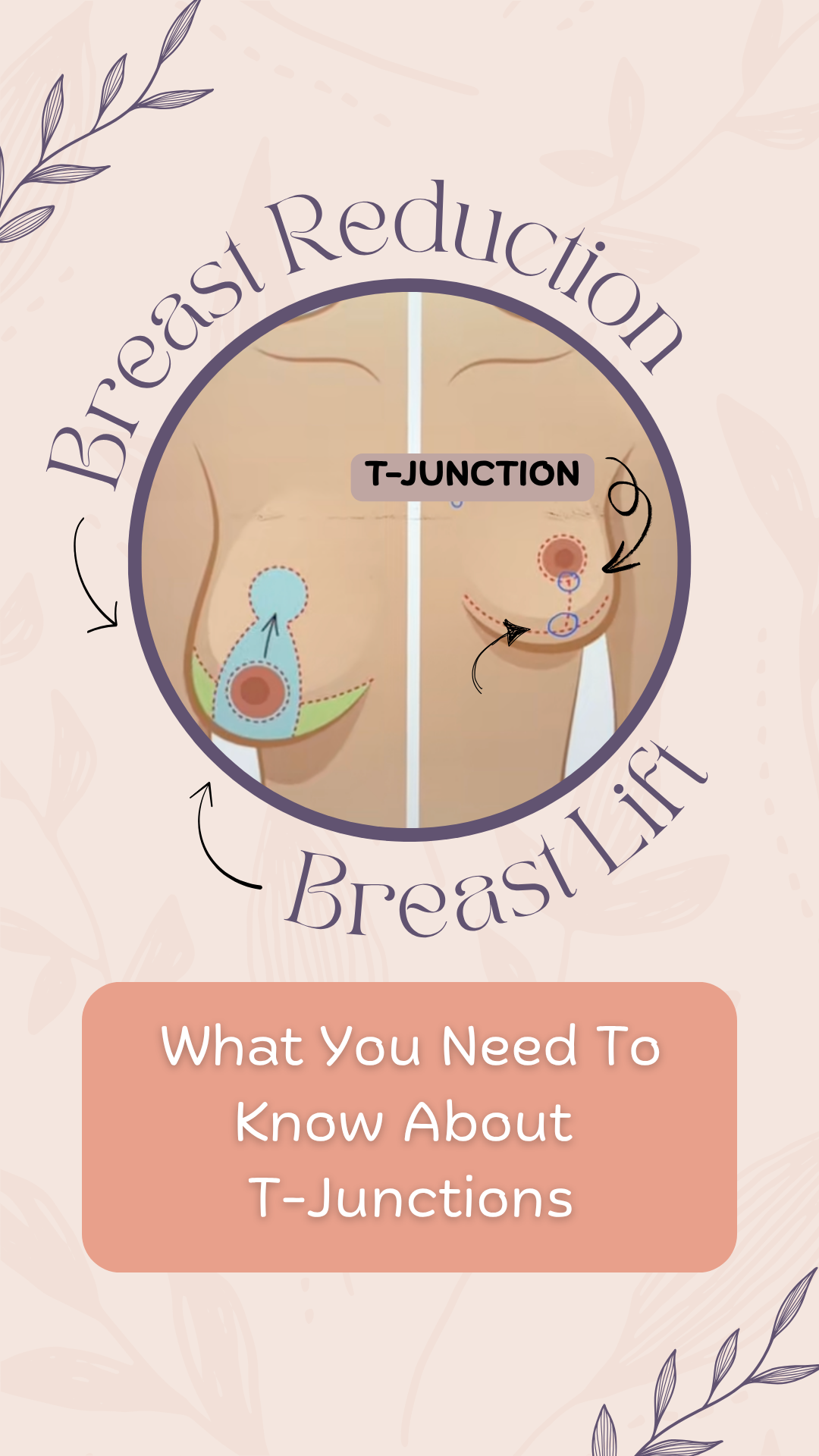
The anchor scar, which is also medically known as an "inverted-T" or "Wise pattern" incision, is characterized by its shape, which resembles an anchor or an inverted letter "T." It is one of the traditional incision patterns used in breast reduction and breast lift surgeries. The incision typically consists of three components: a vertical incision that runs from the bottom of the areola to the crease under the breast, a horizontal incision along the inframammary crease, and a circular incision around the areola (periareolar incision).The anchor scar allows for significant reshaping and lifting of the breast, making it suitable for cases where there is a substantial amount of excess breast tissue and sagging.
The lollipop scar, as the name suggests, resembles a lollipop, with a vertical incision and a circular (periareolar) incision around the areola. The lollipop scar lacks the horizontal incision along the inframammary crease because skin and breast tissue are not removed in this area. While less incisions and scars can be desirable, the trade off is that it makes shortening an elongated breast very difficult.
Dr. Aime generally performs breast lifts and breast reductions with an anchor scar so that the breast can be optimally shaped horizontally and vertically.
Though sharing similarities in surgical technique, these two procedures vary in their intended outcomes. A breast lift, or mastopexy, is undertaken to address the issue of sagging or drooping breasts. Its objective is to elevate and reshape the breasts by repositioning existing breast tissue and eliminating surplus skin and a minor amount of breast tissue. Notably, a mastopexy does not substantially alter the size of the breasts; its primary aim is the restoration of a more youthful and uplifted breast profile.
Conversely, a breast reduction focuses on decreasing the size of the breasts. This procedure is predominantly chosen by individuals with excessively large and burdensome breasts, leading to physical discomfort such as back, neck, or shoulder pain, along with posture issues. While a breast reduction can also result in a lifted appearance, its primary emphasis lies in reducing breast volume and weight.
Regrettably, obtaining insurance coverage for breast reductions has become increasingly challenging over the last decade or so. Many insurance companies now demand the reporting of specific symptoms (such as back/neck pain, difficulty exercising, the need to wear multiple bras, challenges with clothing), observable physical signs (like bra strap grooving), and documented attempts at interventions, including a minimum of six months of NSAID use or engagement in physical therapy. Despite fulfilling these criteria, patients may face insurance denials post-surgery (even after prior authorization) if the removed breast tissue is deemed insufficient. The required amount is determined by body surface area (calculated from height and weight) using the 'Schnur Scale,' establishing the minimum grams of breast tissue to be removed for insurance coverage. For instance, a patient with a height and weight of 5'4" and 150 lbs, resulting in a calculated body surface area of 1.7466 m2, would typically need to have approximately 404 grams of breast tissue removed from each breast for insurance coverage. This equates to about 14 oz or roughly 1.75 cups (equivalent to a grande Starbucks cup). However, this poses a challenge for smaller or more petite individuals, as the mandated removal quantity can leave them with limited breast tissue remaining.
There is no specific minimum age requirement for breast reduction. Minors can undergo a breast reduction with parental approval. While age is not a major concern, it is generally advisable to wait until one is a bit older. This allows individuals to gain a better understanding of their bodies and ensures that their bodies have completed a significant portion of the developmental stage. However, a notable issue is that breasts may continue to grow after the procedure, potentially necessitating another breast reduction. Therefore, it is optimal to wait until a medical professional deems that the breasts have fully developed. The timeline varies for each individual, but typically women are considered fully developed by the age of 18, although some may still experience breast growth into their twenties.
There is no upper age limit for breast reduction surgery. The primary consideration for older patients revolves around the overall health of the individual and whether their body can adequately support the breast reduction procedure. Generally, as long as a patient is in good health, it is okay to proceed with the procedure. The determination of whether one is in "good health" for the surgery is generally made by the surgeon in conjunction with the patient's primary care physician and other physicians (such as cardiologists and anesthesiologists). Older patients are generally required to have pre-operative labs drawn and an EKG performed.
While breast tissue that has been surgically removed does not regenerate, it is possible for the breasts to increase in size again under certain conditions. In rare cases—especially in adolescents or young women who undergo surgery before reaching full hormonal maturity—continued breast growth can occur due to a condition known as juvenile macromastia or virginal hypertrophy. This is believed to be related to an abnormally heightened response of breast tissue to normal hormonal signals, not due to tissue regrowth.
More commonly, weight gain, pregnancy, menopause, or hormonal fluctuations can cause the remaining breast tissue or fat to enlarge. While this doesn’t represent “regrowth” of removed tissue, it may alter surgical results over time.
For most mature patients with stable weight and hormone levels, breast reduction results are long-lasting. If future enlargement occurs, a secondary reduction may be considered.
Breast reduction surgery is not intended as a cancer prevention procedure, but it may be associated with a modest reduction in breast cancer risk. This is because the surgery removes a significant amount of breast tissue, and breast cancer originates in that tissue. Fewer breast cells mean fewer opportunities for abnormal growth, which may contribute to a lower lifetime risk.
However, breast reduction does not eliminate your risk, and it’s important to understand that breast cancer can still develop in the remaining tissue. Routine breast cancer screening, including mammograms, remains essential—especially if you’re over 40, have a personal or family history of breast cancer, or carry a known genetic mutation such as BRCA1 or BRCA2. If you have a strong personal or family history of breast cancer or genetic mutations like BRCA1 or BRCA2, you should discuss this with your surgeon or a breast specialist, as those cases may require different management strategies.
In summary, while breast reduction may slightly lower risk, it does not replace the need for regular screening and monitoring.
While it’s uncommon, suspicious or unexpected findings — including benign tumors, precancerous changes, or even undiagnosed breast cancer — can occasionally be found in the breast tissue removed during a breast reduction. Studies estimate that incidental findings occur in approximately 1–4% of cases, and a smaller percentage of those may be malignant.
That’s why all excised breast tissue is routinely sent to pathology for microscopic evaluation. This process helps ensure that any hidden abnormalities are detected early, even if the patient had no symptoms or abnormal imaging beforehand. In rare cases where something concerning is found, early diagnosis allows for timely treatment or monitoring, which can significantly improve outcomes.
In summary, sending the tissue to pathology is a critical safety step—not just a formality. It adds an extra layer of reassurance and ensures your care is thorough and complete.
Ready to start your transformation?
Whether you’re just beginning to explore your options or have specific goals in mind, we’re here to guide you with expertise and compassion.

Read more articles

Fat Transfer to Breasts
Fat transfer breast augmentation enhances breast size and shape by using your own fat, harvested from other areas of your body, for a soft, natural result.

Breast Revision
Breast revision surgery addresses complications or aesthetic concerns from previous breast procedures, offering improved shape, symmetry, and satisfaction.

Breast Lift
A breast lift (mastopexy) is a surgical procedure that raises and reshapes sagging breasts by removing excess skin and restoring youthful contour and position.

Breast Augmentation
Enhance your confidence and curves with breast augmentation using saline or silicone implants. Personalized, long-lasting results tailored to your aesthetic goals.